Why I often recommend early sacroiliac joint injections
Sacroiliac joint injections can be very effective when done early, typically within 1-10 months of injury. In my experience, a single steroid injection to the SI joint is often curative for this form of pain.
Note: If relief lasts only 3-4 weeks, that pattern often suggests ligamentous laxity. In those cases, I transition to prolotherapy or PRP to provide longer-lasting stabilization.
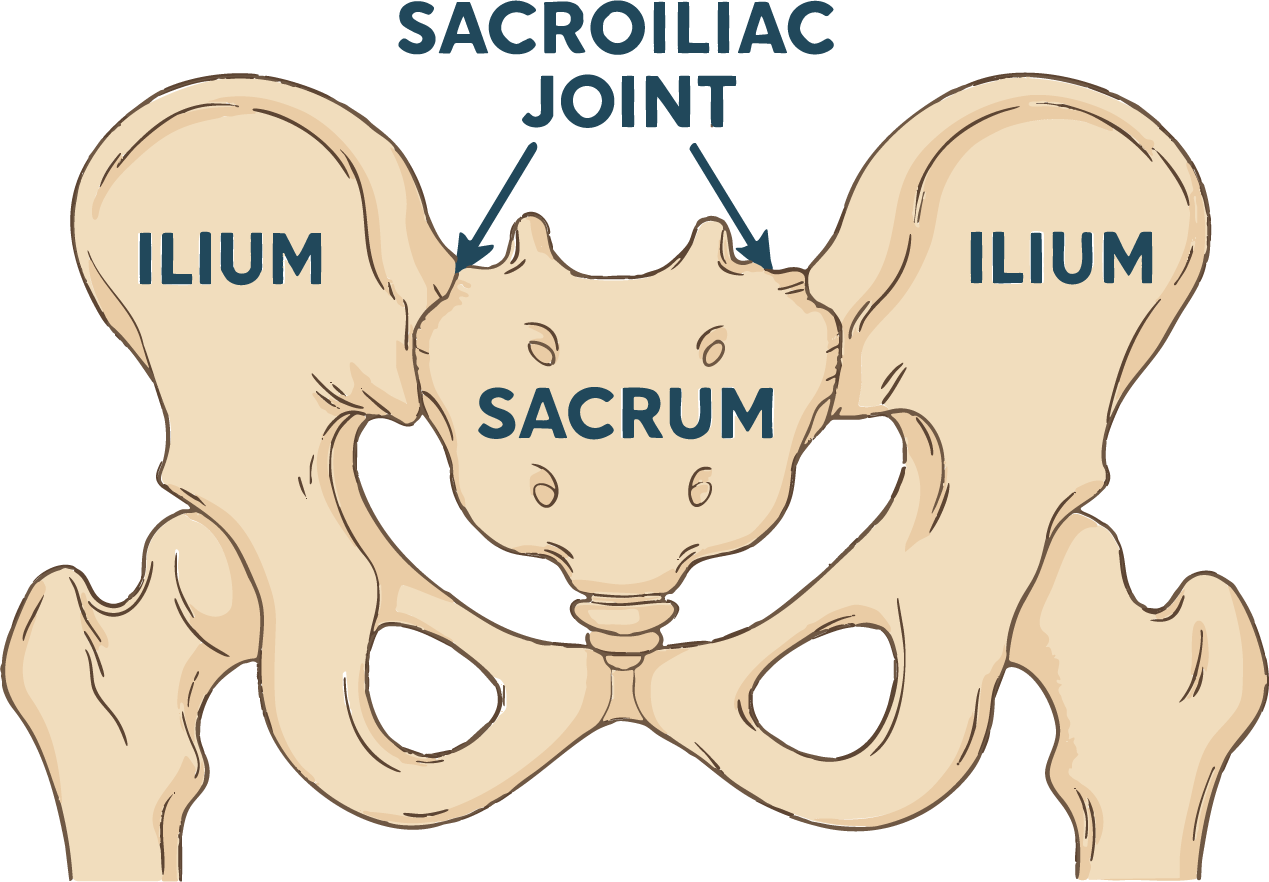
The sacroiliac (SI) joint is where the bottom of the spine (sacrum) meets the hip bones (ilia) on both sides. It is a recognized source of pain after missed steps, slips, or landing on the buttocks.
Crash Mechanics: Vertical Shear
After motor-vehicle collisions, SI pain is common, and I also see psoas reactivity or spasm as part of the same movement pattern. Clinically, SI symptoms often appear when:
- Vehicles are different heights (e.g., car vs SUV)
- The struck vehicle has a tow hitch
The height mismatch imparts vertical shear and torsional loading through the pelvis. This explains why buttock-to-lateral-thigh pain and anterior hip or groin tightness often occur together.
Typical Pain Patterns
Location
Buttock, radiating down the outside of the thigh to the knee.
Triggers
Pain with standing, sometimes sitting. Bending backward often hurts more than forward.
Sensation
Deep ache, burning, or tingling extending down the lateral leg.
Differentiation: Discogenic vs. SI Pain
While literature lists discogenic pain as the most common cause of low back pain, sacroiliac joint involvement appears more frequently in real-world crash mechanics due to seatbelt asymmetry and vertical shear.
Important Distinction: Discogenic pain typically reflects intradiscal disruption (small tears), causing deep, central back pain but rarely leg symptoms. These cases respond best to conservative rehabilitation. Epidural steroid injections usually fail here because the pathology is inside the disc, not a pinched nerve.